Strengthening primary healthcare systems through goood governance

By: Carla Marie L. Asis, Leonila F. Dans and Carol T. Lim
SUMMARY
Good governance is vital in strengthening primary healthcare systems – a building block for universal health coverage. It aligns the system towards goals, coordinates all parts of the system, and provides policy guidance for steering the system. The Philippine Primary Care Studies identified key governance challenges in the implementation of interventions intended to strengthen primary care in urban, rural, and remote health centers in the country. Improvements in implementation, financing, management and coordination, supply and infrastructure, human resources, and community engagement should be undertaken. Recommendations for specific governance issues are outlined in this policy brief.
======================================
ROLE OF GOVERNANCE IN HEALTH SYSTEMS
In 2019, the Universal Healthcare (UHC) Law was passed in the Philippines to improve health equity by strengthening support for primary care services. Although this has provided momentum for the improvement of primary care in the Philippines, implementation has proven to be resource-intensive. Chronic human resource and financial deficiencies are aggravated by uncoordinated, inefficient, and fragmented systems.
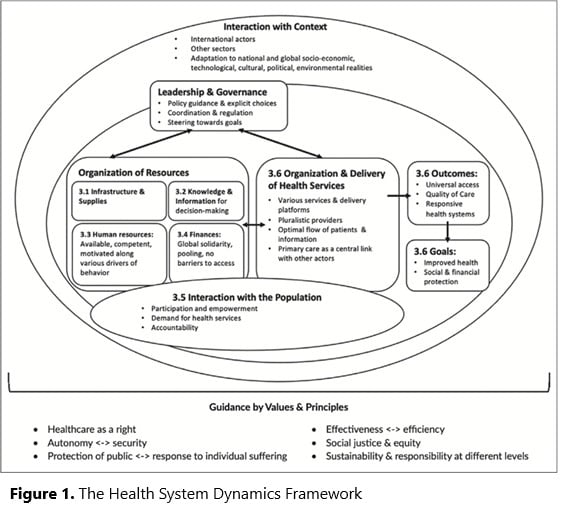
While adequate funding is needed to support the needed health resources, resources allocated to health will not achieve their intended long-term results without attention to good governance. The three main functions of health system governance are: 1) to direct and align the system towards overall goals, 2) to regulate and coordinate all parts of the system, and 3) to provide policy guidance and options for steering the system. This study used the Health System Dynamics Framework (Figure 1), which illustrates the different aspects of the health care system where governance exerts its functions, and where prominent challenges were identified.
GOVERNANCE CHALLENGES IN PRIMARY CARE IN THE PHILIPPINES
The Philippine Primary Care Studies (PPCS) program aimed to strengthen primary care systems in the country. Key governance challenges were identified during the implementation of interventions to strengthen and fund primary care in selected urban, rural, and remote sites. The following six key challenges were identified:
- Establishing a health information system (HIS, a digitized system that aids in evidence-based decisions on health policy)
- Engaging leaders, healthcare staff, and communities
- Assuring efficient financing
- Assuring health workforce sufficiency and competence
- Establishing infrastructure and supply chains
- Planning evaluation and monitoring
PRIORITY HEALTH GOVERNANCE RESPONSES
Recommendations for specific governance issues are outlined in the table below.
| Challenges | Recommendations |
| ESTABLISHING A HEALTH INFORMATION SYSTEM | |
| Resistance to a digitized records system | ● Develop an EHR system in collaboration with end-users and following facility workflows
● Automate routine tasks such as censuses and reports to incentivize the use of the EHR ● Regularly train facility staff to prevent the need for third-party encoders ● Link payments to regulatory measures such as the use of the ICD-10, PNDF, and DPRI |
| Ambiguous facility workflow | ● Design an EHR system suitable for the facility workflows; shared decision-making should be encouraged between developers and users
● Address misconceptions to improve EHR acceptance |
|
Duplication of medical records |
● Develop biometric identification systems to limit record duplication |
|
Responsiveness to EHR troubleshooting concerns |
● Outsource IT development to ensure efficient debugging, development, and maintenance of HIS program and infrastructure[4] [5] |
| Interoperability with pharmacy, lab, and other facilities | ● Implement a unified HIS for primary care centers within designated areas
● Improve inter-and intra-departmental awareness on system updates to ensure databases are backed up |
| HIS infrastructure | ● LGUs must seek internet service providers such as satellite providers to support the needs of primary care facilities
● LGUs must proactively incorporate the establishment of sustainable IT infrastructure in their respective financial investment plans |
| Hardware security | ● Store HIS hardware in secure locations and limit access to authorized personnel only
● Mitigate the risk of property loss or damage by installing locks, securing offices, and implementing tracking measures ● Enjoin patients to protect the equipment used in their own healthcare |
| Data security | ● Regularly train facility staff on data privacy and the need to maintain patient confidentiality |
|
ENGAGING LEADERS, HEALTHCARE STAFF, AND COMMUNITIES |
|
| Lack of engagement with leaders and healthcare staff | ● Consult with experts and figures across a multitude of disciplines beyond the clinical sciences, such as public health, economics, engineering, communication arts, social sciences, statistics, information technology, among many others
Conduct early engagement with community leaders, health officers, key decision-makers, and institutions (e.g., DOH and PhilHealth)
|
| Lack of engagement with community members and target beneficiaries | ● Endear the public with the concept of primary care through town hall meetings, videos, brochures, posters, and similar content
● Introduce the concept of risk-sharing in the local language (e.g., paluwagan) and context familiar to target beneficiaries |
|
ASSURING HEALTH WORKFORCE SUFFICIENCY AND COMPETENCE |
|
| Undermanned primary care centers |
● LGUs and HCPNs must collaborate to improve the patient: provider ratio, near levels prescribed by the WHO ● Legislation is needed to override current personnel salary capitations and allow the hiring of an adequate number of PCPs ● Encourage HCPNs to recruit providers and practitioners residing within the vicinity of facilities to improve retention HCPNs must provide performance-based incentives to motivate better performance in healthcare delivery
|
| Continuing professional development in resource-limited settings | ● Regularly train PCPs with sufficient medical resources such as UpToDate® to enhance knowledge access and retention |
| Demoralized primary care workforce |
● LGUs and provincial health units must host motivational workshops about the crucial role of primary care in the Philippines ● Ensure sustained dialogue between system implementers, policymakers, and frontline workers
|
|
Unclear delineation of roles |
● HCPNs must clarify the roles and expectations from doctors, nurses, midwives, BHWs, and other facility staff to facilitate teamwork |
|
CREATING WELL-ESTABLISHED INFRASTRUCTURE AND SUPPLY CHAINS |
|
| Procurement systems remain inefficient due to extensive bureaucracy | ● LGUs must actively engage the private sector to support the logistical limitations of public healthcare facilities
● LGUs must encourage private sector engagement to improve resource supply and service efficiency ● Credible third-party agencies must be permitted to independently monitor the health care financial expenditures of LGUs |
|
EVALUATION AND MONITORING |
|
| Policymakers focus on vertical or disease-specific outcomes | ● Explore horizontal outcomes such as overall patient satisfaction, utilization, hospitalization, and out-of-pocket expenses |
| Non-interest in health provider outcomes
|
● Monitor provider satisfaction and retention, knowledge, quality of care, and EHR satisfaction
|
| Inability to make actuarial predictions | ● Conduct regular costing studies |
| Bureaucratic delays impede proper monitoring and evaluation |
● Monitor administrative efficiency ● Standardize processes, establish autonomy, and monitor compliance to Anti Red Tape Act |
HIS, Health Information System; EHR, Electronic health record; ICD-10, International Classification of Diseases-10; PNDF, Philippine National Drug Formulary; DPRI, Drug Price Reference Index; IT, Information technology; LGU, Local government unit; HCPN, Healthcare provider network; PCP, Primary care provider; BHW, Barangay health worker
THE PATH FORWARD
Most health facilities can transition into a strengthened primary care system provided improvements in implementation, financing, management and coordination, supply and infrastructure, human resources, and community engagement are achieved. Routine decision-making by multiple actors within the governance structure can significantly impact primary care systems and their resultant outcomes. As such, good governance lays central in strengthening primary care in the Philippines and improving outcomes for providers and patients alike.
===========================
Citation
Bernal-Sundiang N, De Mesa RYH, Marfori JRA, Fabian NMC, Calderon YT, Dans LF, Rey MP, Sanchez JT, Galingana CLT, Catabui JT, Paterno RPP, Co EEA, Dans AML. Governance in Primary Care Systems: Experiences and Lessons from Urban, Rural, and Remote Settings in the Philippines. Acta Med Philipp [Internet]. 2023Mar.28;57(3). Available from: https://actamedicaphilippina.upm.edu.ph/index.php/acta/article/view/4834